Frequently Asked Questions
The following FAQs should help address your questions about North Charleston Sedation Associates and your anesthesia bill. If they don’t, please contact us directly for assistance.
- Just had your procedure? Now what?
- Do I need to file anything with my insurance provider?
- My insurance sent me a check, what should I do?
- What insurance providers do you participate with?
- What if my insurance provider participates with the endoscopy center but not with North Charleston Sedation Associates?
- How to read your patient statement
- How to read your Explanation of Benefits (EOB)
- How much does anesthesia cost?
- Why did I receive multiple bills for the same procedure?
- When is payment due?
- What forms of payment do you accept?
Just had your procedure? Now what?
Ideally, your insurance will process everything correctly the first time around so you won’t need to worry about anything. In the unfortunate case that they do not, we will send a letter with a statement and a form to sign so that we can assist in getting your balance reduced or eliminated.
Do I need to file anything with my insurance provider?
As a courtesy to you, the bills for your anesthesia services will be filed to your insurance company. We have accepted assignment of these benefits and your insurance company should send the payment directly to our office. If we have a secondary insurance on file for you, we will file a claim for the amount not paid by your primary insurance. If there is no secondary insurance on file, then we will send you a bill for the co-payment due as determined by your insurance company.
My insurance sent me a check, what should I do?
If your insurance company sends payment directly to you, you may either endorse the check OR write a personal check for the amount received and send it to the address listed below.
North Charleston Sedation Associates
P.O. Box 738519
Dallas, TX 75373-8519
What insurance providers do you participate with?
We accept any insurance that the facility where you are having the service accepts. Because we are an ancillary provider, we typically do not need to contract separately with your insurance to be processed in-network (several BCBS plans are the exception). We contract with all federal (Medicare, Tricare) and state plans (Medicaid).
In the event that we are not a participating anesthesia provider within your insurance plan, we will work with your insurance company to insure that you are not penalized for our non-participating (out-of-network) status. The maximum amount that you will owe will be your participating (in-network) benefit rates. Please contact us if you have ANY concerns.
What if my insurance provider participates with the endoscopy center but not with North Charleston Sedation Associates?
We accept any insurance that the center accepts. Anesthesia providers are considered ancillary providers and because of this, regardless of our network status, most insurances will process the claim as though we are in network. Plan types typically have a plan provision that states ancillary providers (such as radiologists, anesthesiologists and pathologists) will be processed under your in-network level of benefits as long as the facility is in-network. On occasion, the insurances do not process payments correctly the first time around so we may need your assistance by signing a form in order to reduce or eliminate your responsibility. We will contact you if this is necessary.
How to read your patient statement
Column 1: Dates
The first line item will be the date of service. All other line items will be the date a payment or adjustment was taken.
Column 2: Description of service
This is where you see the service billed for, the provider who performed the service, and any information regarding payments and adjustments.
Column 3: Financial amounts
These are the costs for what is described in column 2.
Columns 4 & 5: Balances
These are any balances on your account to be paid by your insurance (Column 4) or you (Column 5).
We advise you to pay close attention to the message at the bottom of the statement. This message often provides important information such as to whether the balance can be further reduced, or what to do in the case you receive a check from your insurance provider that needs to be forwarded so that an adjustment can be made.

How to read your Explanation of Benefits (EOB)
Your EOB is plan specific, so please contact us directly so that we can address your specific questions over the phone. If we are notified of a denial, we will send you notices explaining your benefits and appeal rights. These letters are insurance specific and typically explain what needs to be done to have the balance reduced or eliminated.
Your EOB may identify:
- The patient and the service provided
- The amount charged by the provider
- The amount of the charges that are covered and not covered under your plan
- The amount paid to your provider
- The amount you’re responsible for
Remember that your EOB is not a bill, it just explains what was covered by insurance. Your provider may bill you separately for any charges you’re still responsible for. You may receive a few EOBs over time if your claim is being appealed.
Sample EOB
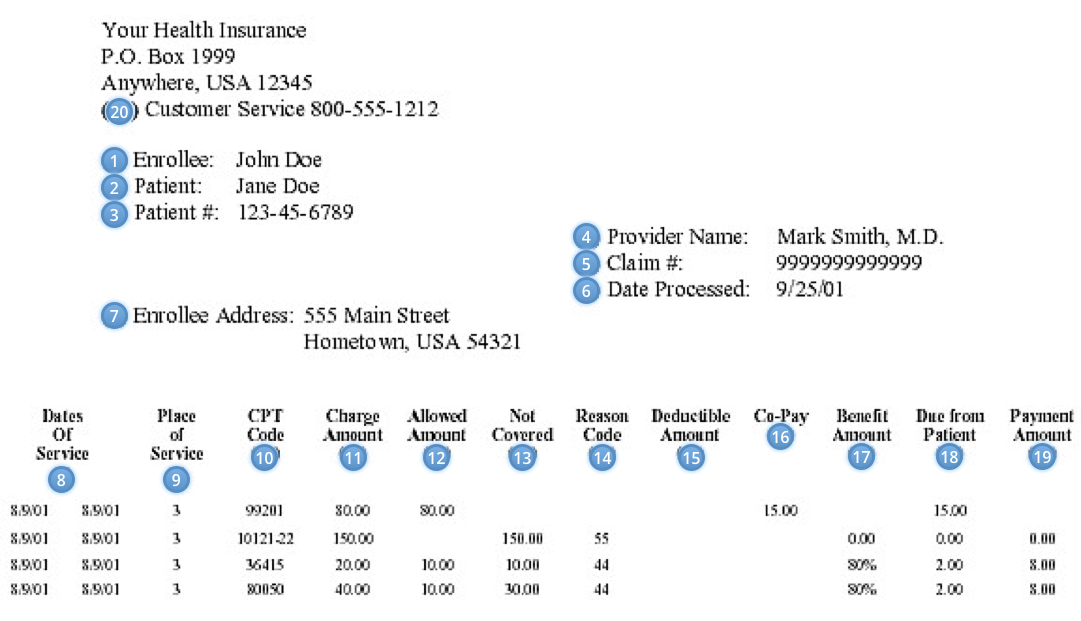
- Enrollee Name: Identifies the policyholder. This is usually the name of the person who carries the insurance.
- Patient: Identifies the patient.
- Patient #: This serves as an identification number for the patient.
- Provider Name: Identifies the name of the doctor or center that is billing for the services. Verify services were actually rendered by the provider listed.
- Claim #: This is a number assigned to the claim by the insurance company to identify the claim in their computer system.
- Date Processed: Indicates the date on which the claim is processed.
- Enrollee Address: Indicates the address of the enrollee; this should be verified with each claim. Wrong addresses can cause problems in claims payment.
- Dates of Service: Indicates the dates of service on which the service was rendered.
- Place of Service: Indicates the location the service was rendered. This is important as some services are only covered in specific locations.
- CPT Code: This identifies the service performed. This code is universal and dictates the payment allowances.
- Charge Amount: Amount charged by provider of service.
- Allowed Amount: Amount determined by a preset schedule of “usual and customary” (UCR) charges. Amount is usually determined by geographic location of provider.
- Not Covered: Amount not included in the allowed amount; usually this is the amount deemed over the usual and customary allowance. In most incidences, the patient is responsible for the overage.
- Reason Code: This is an explanation of why a service has been has denied, or why an amount is not covered.
- Deductible: This reflects the amount the patient must pay prior to having benefits paid. Amounts that are not covered are not applied to the deductible. Generally, each patient will have his or her own deductible to meet. Deductibles may be required for both participating and not participating services; refer to the schedule of benefits.
- Co-Pay: A minimal amount required from the patient when seeking services from a provider. Usually the patient is only responsible for copayments at a participating provider.
- Benefit Amount: This is the percentage at which the amount covered will be paid. The percentage paid will be determined by the schedule of benefits. Generally, participating providers will be paid at a higher level; non-participating providers will be paid a lower level.
- Due from Patient: This is the amount the patient is responsible for paying to the provider. This generally includes the co-insurance amount, deductible and may or may not include the amount over the UCR. If the amount over the UCR is not included, the patient needs to verify if the provider of service will write the amount off. If the provider of service will not write the amount off, the patient is responsible.
- Payment Amount: The amount paid to the provider.
- Customer Service: This is the number used to contact customer service.
How much does anesthesia cost?
Providing an estimate is quite difficult for anesthesia because processing is based on time or charged amount and is plan specific. If your service is a screening procedure, most plans will cover this at 100% of their allowed amount. Exceptions to this include some BCBS plans and grandfathered commercial plans. We are happy to assist when possible, however, due to the number of insurance plans, we suggest that you contact your insurance company if you have a specific question regarding your individual coverage. If you are not covered by your insurance and required information regarding self-pay rates, please contact us.
Why did I receive multiple bills for the same procedure?
The procedure you had has 3 (three), possibly 4 (four) separately billable components that consist of:
- The professional services of the gastroenterologist
- The professional & medical services of the anesthesiologist / anesthetist
- The facility fee (for use of the surgery center)
- Pathology/lab fees (if you have polyps removed or biopsies taken)
Each of these services is provided under separate entities/companies and cannot answer billing questions for the other, so please contact the appropriate company for your questions. We can address all questions related to #2.
When is payment due?
Payment is due within 10 days of receipt of the statement, however we do accept payments in installments. If you would like to pay in installments, please notify us by contacting us directly.
What forms of payment do you accept?
We accept credit cards and checks. You can pay online using our payment portal.
If you would prefer to pay over the phone, please contact us at (888) 717-5383.
Alternatively, you can mail a check to:
North Charleston Sedation Associates
P.O. Box 738519
Dallas, TX 75373-8519
 (888) 717-5383
(888) 717-5383